
Glaucoma is a spectrum of disease diseases that caused optic nerve damage, resulting in visual loss and potentially blindness.
Some of the diseases or underlying conditions that can contribute to the development of glaucoma, include the following:
Types of Glaucoma
There are several types of glaucoma.
Risk Factors for Glaucoma
There are several factors that contribute to the risk of developing glaucoma. They include some of the following:
Symptoms of Glaucoma
Glaucoma symptoms depend on the type of glaucoma and how advanced it is. In the early stages, most types have no noticeable symptoms, which is why regular eye exams are critical.
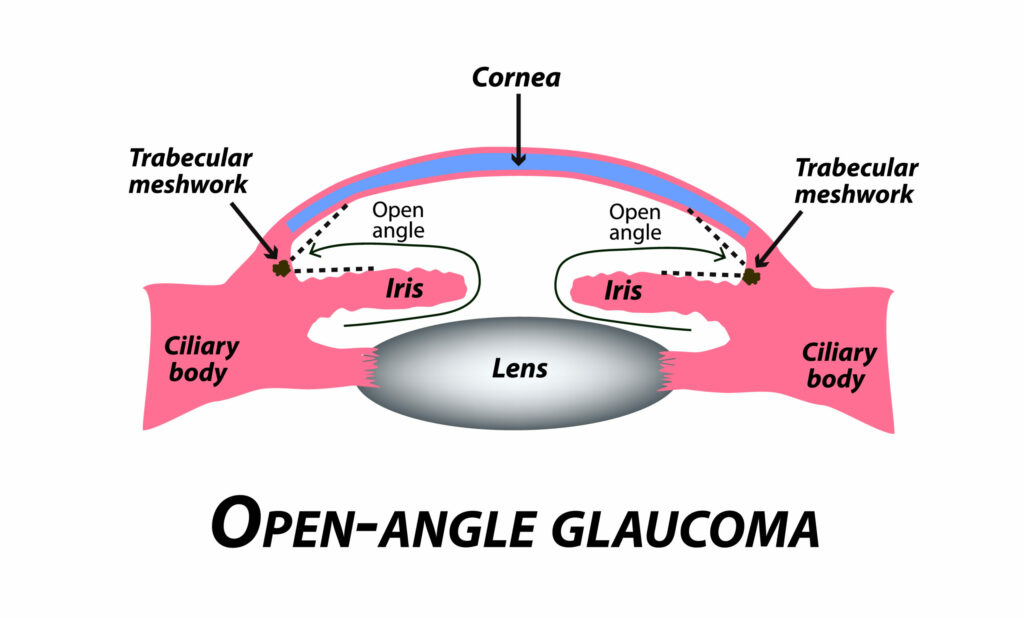
Open-Angle Glaucoma
(Most Common Type)
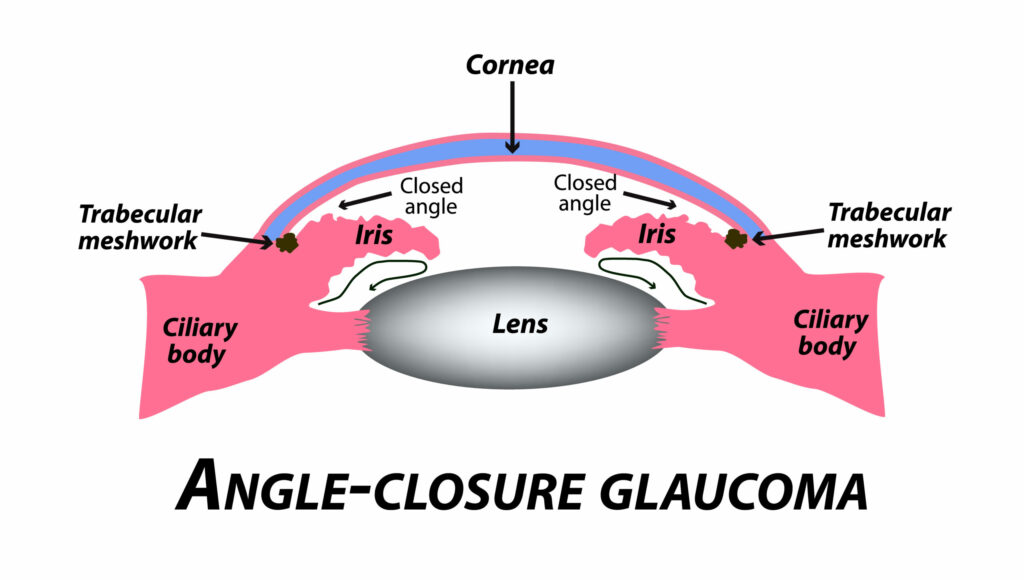
Angle-Closure Glaucoma
(Less Common, More Sudden & Severe)
Diagnosis of Glaucoma
To diagnose glaucoma, eye doctors perform a comprehensive eye exam that includes:
Treatment of Glaucoma
Although there is no cure for glaucoma, treatment can slow or stop progression and preserve vision. Early diagnosis is vital to prevent object nerve damage.
Medications
Prescription eye drops or oral medications help:
Laser Surgery for Glaucoma
Laser procedures improve fluid drainage or reduce fluid production. Options include:
Surgical Treatment for Glaucoma
When medications and laser treatments are insufficient, surgical intervention can help lower intraocular pressure and prevent further optic nerve damage. The surgical options offered at our practice include:
Minimally Invasive Glaucoma Surgery (MIGS)
MIGS procedures provide effective pressure reduction with less risk and a faster recovery compared to traditional glaucoma surgeries. We offer:

MIGS procedures are often combined with cataract surgery to enhance results.
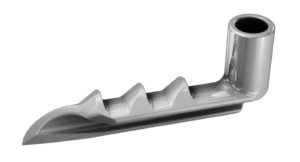
Trabeculectomy (With or Without EX-PRESS® Shunt)
Trabeculectomy is a gold-standard glaucoma surgery that creates a new drainage channel for fluid to exit the eye.
Tube Shunt Surgery (Ahmed Valve and Other Devices)
For moderate-to-severe glaucoma, a tube shunt can be implanted to divert fluid and lower pressure.
Each surgical option is tailored to the severity of glaucoma, patient anatomy, and long-term goals.
Injectables
Durysta®: A Tiny Implant That Helps Control Eye Pressure
If you’re living with open-angle glaucoma or ocular hypertension, managing eye pressure daily can feel like a constant task. Durysta® offers a breakthrough solution: it’s the first and only FDA-approved dissolvable implant that delivers glaucoma medication directly inside the eye—no need for daily drops.
What Is Durysta®?
Durysta is a prescription drug delivery system that slowly releases medication (bimatoprost) over time to lower intraocular pressure (IOP) in patients with open-angle glaucoma or high eye pressure. It’s a tiny, biodegradable implant—smaller than the “I” in the word LIBERTY on a dime! Once placed inside the eye, it gradually dissolves on its own, delivering precise dosing automatically for several months.
Note: Durysta is currently approved as a one-time treatment per eye.
How the Procedure Works
The Durysta implant is placed during a quick, in-office procedure by your eye doctor. Using a specialized applicator, we insert the implant directly into the front chamber of your eye. There are no incisions or stitches, and most patients find the experience similar to a standard eye injection.

*Dime enlarged to show detail.
Once in place, the implant begins releasing medication to reduce pressure inside the eye. The entire process takes just a few minutes.
How Long Does Durysta Last?
In clinical studies, Durysta lowered eye pressure for up to 15 weeks with just one implant. While results can vary slightly from patient to patient, many people enjoy several months of consistent IOP control from a single treatment.
This makes Durysta an especially valuable option for patients who:
Benefits of Durysta
Are There Side Effects?
As with any eye procedure, there are some potential side effects. In clinical trials, the most common side effect was eye redness. Others included:
We’ll review your full medical and ocular history to determine if Durysta is a safe and effective option for you.
Is Durysta Right for You?
Durysta isn’t for everyone, but it may be a great choice if you’re looking for long-term pressure control without the hassle of daily drops. If you’ve been diagnosed with open-angle glaucoma or ocular hypertension, we’ll discuss whether you’re a good candidate during your consultation.
Let’s talk about the right treatment plan for your eyes—and your lifestyle.
